VENUSCANCER: A Worldwide View of Breast, Cervical & Ovarian Cancer
Speed-read
- Given the many global differences when it comes to cancer, scientists have conducted the largest-ever analysis of data from more than 275,000 women in 39 countries (across all continents), revealing patterns in breast, cervical, and ovarian cancer. The VENUSCANCER project, funded by the European Research Council, provides the first global picture of care patterns for the three most common cancers in women.
- One in five women with breast or cervical cancer in low- and middle-income countries is diagnosed with cancer at an early stage, compared with more than one in three in high-income countries. Advanced cervical cancer was less than 15% in most countries worldwide. Ovarian cancer continues to be diagnosed at an advanced stage.
- In sub-Saharan Africa overall, fewer than 3% of women with a known stage were recorded to have an early-stage breast cancer. In South Africa (Eastern Cape) and Mongolia, mastectomy was the only treatment option offered to women diagnosed with early-stage breast cancer.
- Around 30–40% of cervical tumors were diagnosed as early-stage in most HICs. Less than 1% of cervical cancers were diagnosed at an early stage in South Africa (Eastern Cape), but this proportion was much higher in Romania (Cluj; 22.5%), Thailand (25.3%), Georgia (29.2%), and Russia (36.9%).
- Most women with an early-stage ovarian tumor (≥98%) were treated with surgery in most HICs, but this proportion was slightly lower in Germany (Hamburg; 86.4%), Italy (87.9%), and Spain (85.0%). The proportion of women diagnosed with metastatic ovarian cancer who received both surgery and chemotherapy ranged from 15.4% in Portugal to 53.2% in the USA. The median time from diagnosis of ovarian cancer to surgery for early-stage tumors was slightly less than 1 month in the USA, Belgium, and Norway; 1–2 months in Italy, Spain, Estonia, and Puerto Rico; and over 2 months in Portugal and Canada.
- Findings highlight several key messages for governments and policymakers worldwide. Prompt access to optimal treatment for breast, cervical, and ovarian cancers was available in most countries for early-stage tumors; therefore, efforts to promote improvement of early cancer detection should continue, both in HICs and LMICs. An increased number of radiotherapy centers and trained staff in LMICs, together with an increase in the coverage of public health insurance to include radiotherapy for economically disadvantaged women in some HICs, would improve consistency with treatment guidelines involving radiotherapy. International agreement on clinical guidelines is crucial, but they need to be tailored to local needs and resources, simplified, and made available in local languages.
Breast, cervical, and ovarian cancers claim hundreds of thousands of lives each year. In 2022 alone, an estimated 2.3 million women worldwide were diagnosed with breast cancer, and 670,000 died. These alarming numbers highlight the urgent need to understand how women with these cancers are diagnosed and treated worldwide.
The VENUSCANCER: The first global picture of how breast, cervical, and ovarian cancers are diagnosed and treated
Given the many global differences when it comes to cancer, scientists have conducted the largest-ever analysis of data from more than 275,000 women in 39 countries (across all continents), revealing patterns in breast, cervical, and ovarian cancer.
This month, the team of international scientists presented the first global picture of major differences in care for women with these cancers. The results are published in the study “Global variation in patterns of care and time to initial treatment for breast, cervical, and ovarian cancer from 2015 to 2018 (VENUSCANCER): a secondary analysis of individual records for 275 792 women from 103 population-based cancer registries in 39 countries and territories.”
“We have created the largest population-based, high-resolution database for the three most common cancers in women, including detailed information on stage at diagnosis, staging procedures, treatment, and biomarkers,” they wrote in the study.
We spoke with Claudia Allemani, Lead Author and Principal Investigator of the VENUSCANCER study, and Professor of Global Public Health at the London School of Hygiene & Tropical Medicine (LSHTM).
CONCORD and VENUSCANCER: Explained in the study
Ten years ago, in 2015 to be exact, the CONCORD program established a global surveillance of cancer survival trends from 1995 to 2009 (CONCORD-2), documenting large global differences in survival trends for most major cancers in men and women. Then, CONCORD-3 updated survival trends to 2000-14; the differences in survival still existed.
The VENUSCANCER project, included in the CONCORD program, is designed to develop a better understanding of the reasons underlying international inequalities in survival among women with breast, cervical, or ovarian cancer. The VENUSCANCER study used data from 322 cancer registries that had previously contributed to the CONCORD program, collecting information on breast, ovarian, and cervical cancer. As scientists point out in the study, the registries collect basic patient data, including age, sex, place of residence, tumor type, and stage, while more detailed data on therapy, biomarkers, comorbidities, and lifestyle are still not routinely collected in most countries.
VENUSCANCER analyzed data from cancer registries worldwide. For high-income countries (HICs), only registries with ≥70% complete high-resolution stage and treatment data were included, while in Low- and Middle-Income Countries (LMICs), all registries were included. They called for the registration of detailed (“high resolution”) data from the medical records of women diagnosed with breast, ovarian, or cervical cancer in the period 2015-2018. These data include disease stage, staging methods, tumor grade, biomarkers, first-line treatment, dates of treatment, comorbidities, and lifestyle.
The data were standardized according to the ICD-O tumor classification and different staging systems (TNM, SEER, FIGO). The analysis included the distribution of disease stages, the compliance of therapy with international guidelines (ASCO, ESMO, NCCN), and the time from diagnosis to treatment. For all three cancer types, logistic regression was used to estimate the probability of patients receiving treatment according to guidelines, comparing HICs and LMICs, while controlling for age and tumor type.
To ensure consistency in data collection, three comprehensive questionnaires on registration practices were developed. The call for participation in the project was sent on 21 December 2019. The deadline for data submission was originally 30 June 2020, but was extended several times due to the COVID-19 pandemic. The pandemic had different timelines in different parts of the world, so data collection lasted from January 2020 to January 2025. In collaboration with the Idaho Cancer Registry (USA), a SAS program was developed to convert data from the North American format (NAACCR) to the VENUSCANCER protocol, facilitating collaboration with US and Canadian registries. All data are anonymized, submitted via the secure CONCORD platform, and stored, cleaned, and analyzed at the London School of Hygiene & Tropical Medicine.
“In this article, the first from the VENUSCANCER project, we aimed to assess the worldwide variation in patterns of care and time to initial treatment for women with breast, cervical, and ovarian cancer. Separate analyses will be conducted for each cancer to assess whether inequalities in survival from women’s cancers are attributable to differences in disease biology between populations or to patterns of care,” the scientists wrote in the study.
The VENUSCANCER project, funded by the European Research Council, provides the first global picture of care patterns for the three most common cancers in women.
Of the 322 registries invited to participate in the study, 103 contributed high-resolution data for a single year of incidence during 2015–18
“Of the 21 cancer registries in LMICs that were offered financial support to contribute to the VENUSCANCER project, we succeeded in supporting only 11 registries in Uganda (Kampala), Nigeria (Ibadan), South Africa (Eastern Cape), Brazil (São Paulo), Colombia (Cali), Ecuador (Quito), Mongolia, Georgia, Thailand (Chiang Mai and Lampang), and Romania (Cluj). Golestan (Iran) could not receive financial support from the UK due to international sanctions. Registries in Argentina (Mendoza), Brazil (Aracaju, Jaú, and Porto Alegre), Cuba, and Russia (Arkhangelsk) could not open an international bank account. Bulgaria was experiencing political problems that led to the closure of the registry. Trivandrum (India) and Jakarta (Indonesia) could not accept this commitment. Despite the financial support, São Paulo (Brazil) could not contribute adequate data because withdrawal of municipal funding led to closure of the registry in 2022. Cali (Colombia) only provided minimal data.”
Results and some data from the study are presented
“Cuba submitted national data for ovarian cancer; however, for breast cancer, only data for the provinces of Villa Clara (approximately 7·0% of the national population), Pinar del Río (5·3%), and Matanzas (6·4%) were submitted. For some registries in France and Italy, we also accepted data for 2012, because clinical and therapeutic guidelines had not changed much between 2012 and 2018. Cancer stage at diagnosis was known for 214,758 (77·9%) women from 93 registries in 38 countries or territories (23 HICs and 15 LMICs). Australia did not provide data on stage,” as stated in the study.
The results show that one in five women with breast or cervical cancer in low- and middle-income countries is diagnosed with cancer at an early stage, compared with more than one in three in high-income countries. The results also show variations in the stage of the disease at diagnosis, but also in the type of treatment. Metastatic breast cancer accounted for less than 10% in most HICs, but was more common in LMICs, ranging from 2% to 44%. Advanced cervical cancer was less than 15% in most countries worldwide. Ovarian cancer continues to be diagnosed at an advanced stage.
Breast cancer
- In HICs, almost all breast cancer tumors (98–100%) were microscopically verified.
- Metastatic breast cancers were rare in the UK and Puerto Rico (<1%), but occurred in over 9% of breast cancer cases in Martinique, Estonia, and Liechtenstein.
- The median time between diagnosis of breast cancer and breast-conserving surgery for early-stage tumors in women living in HICs was less than 1 month in Belgium, Estonia, Germany (Hamburg), Liechtenstein, Norway, Switzerland, and the UK; 1–2 months in Spain, Slovenia, Canada, the USA, and Puerto Rico; and around 3 months in Portugal.
- In sub-Saharan Africa overall, fewer than 3% of women with a known stage were recorded to have an early-stage breast cancer.
- In South Africa (Eastern Cape) and Mongolia, mastectomy was the only treatment option offered to women diagnosed with early-stage breast cancer.
- Across LMICs, the median time between diagnosis of breast cancer and breast-conserving surgery in early-stage tumors was up to 1 month in Romania (Cluj), Russia (Arkhangelsk), and Thailand; 1–2 months in the occupied Palestinian territory (Gaza), and Brazil; and up to 4 months in Colombia.
Cervical cancer
- Across HICs, almost all cervical tumors were microscopically verified (97–100%), but this proportion was slightly lower in Estonia (94.0%). Not all countries or territories routinely collect information on in situ tumors. The proportion of in-situ tumors was provided only by Montana (89.5%) in the USA, Newfoundland and Labrador (91.1%) in Canada, and the Milan Cancer Registry (82.7%) in Italy.
- Around 30–40% of cervical tumors were diagnosed as early-stage in most HICs, but the proportion of early-stage tumours was as low as 15·0% in Martinique and over 40% in Denmark (42·0%) and the USA (42.3%), New Zealand (43.2%), Norway (46.0%), the UK (46.8%), South Korea (52.2%), and Canada (60.1%). The proportion of women diagnosed with advanced cervical cancer was generally around 13–15%, but as low as 5% in Denmark and Slovenia and as high as 23% in Estonia.
- For early-stage tumors, at least 85% of women diagnosed with cervical cancer were treated with surgery in most HICs, with a range from 65.9% in Northern Ireland to 97.5% in Slovenia.
- Across LMICs, almost all cervical tumors were microscopically verified (96–100%), but this proportion was slightly lower in Uganda (Kampala; 79.8%), Iran (Golestan; 85.2%), Georgia (87.0%), and Mongolia (92.5%).
- Less than 1% of cervical cancers were diagnosed at an early stage in South Africa (Eastern Cape), but this proportion was much higher in Romania (Cluj; 22.5%), Thailand (25.3%), Georgia (29.2%), and Russia (36.9%).
- Up to 6.0% of cervical cancers were diagnosed at an advanced stage in Nigeria (Ibadan), Russia, and Romania (Cluj), compared with 31.4% in Ecuador (Quito).
- Tumors were mostly treated with simple hysterectomy in Uganda (Kampala; 75%), whereas radical hysterectomy was the most common treatment in South Africa (Eastern Cape).
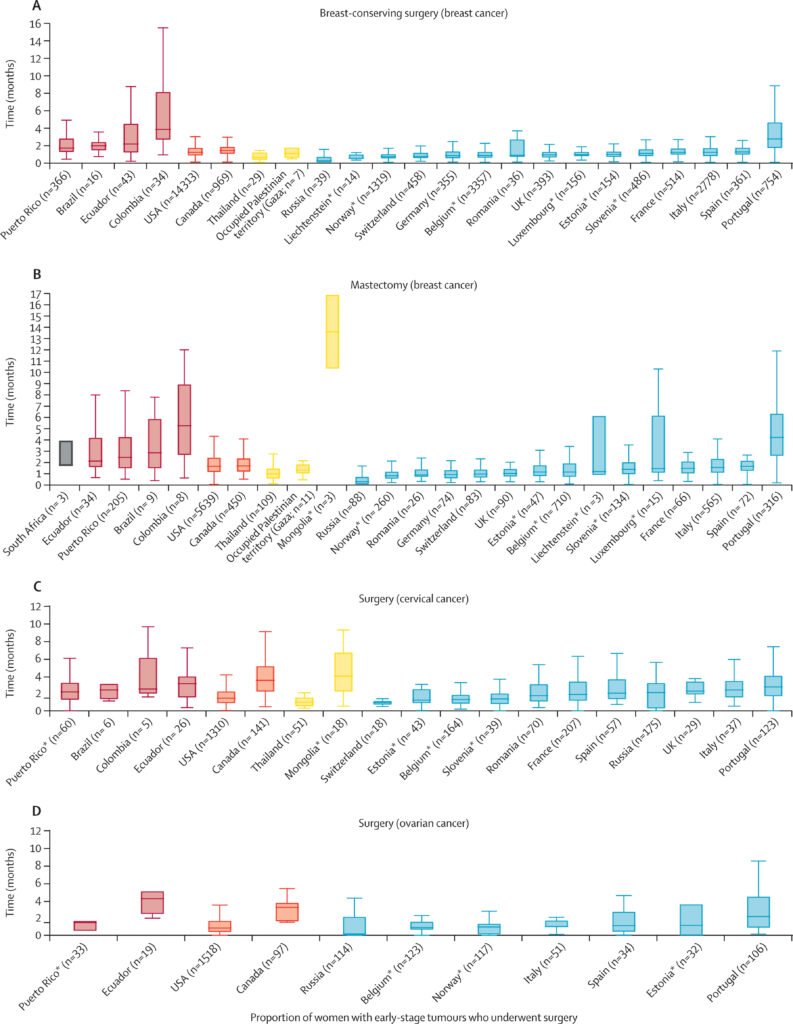
Study: Median time between diagnosis and surgery in women with early-stage breast, cervical, or ovarian cancer
Ovarian cancer
- The proportion of ovarian tumors with a known stage was around 74% in Germany (Hamburg; 74.1%), Ireland (73.9%), and the Netherlands (73.7%), but over 80% in most HICs, and above 90% in Puerto Rico, Canada, the USA, Estonia, Norway, Portugal, Spain, Switzerland, and New Zealand. Early-stage tumors ranged from 14.5% in Belgium and Denmark to 23% in Norway (22.9%) and Portugal (23.0%).
- Most women with an early-stage ovarian tumor (≥98%) were treated with surgery in most HICs, but this proportion was slightly lower in Germany (Hamburg; 86.4%), Italy (87.9%), and Spain (85.0%).
- The proportion of women diagnosed with metastatic ovarian cancer who received both surgery and chemotherapy ranged from 15.4% in Portugal to 53.2% in the USA.
- The median time from diagnosis of ovarian cancer to surgery for early-stage tumors was slightly less than 1 month in the USA, Belgium, and Norway; 1–2 months in Italy, Spain, Estonia, and Puerto Rico; and over 2 months in Portugal and Canada.
- The proportion of early-stage tumors ranged from 4.0% in Mongolia to 26.8% in Russia; that of metastatic stage ranged from 14% in Romania (Cluj; 14.0%) and Russia (13.8%) to 88.5% in Cuba.
- The median time between diagnosis of ovarian cancer and surgery for early-stage tumors ranged from less than 1 month in Russia to over 4 months in Ecuador (Quito).
“Our findings highlight several key messages for governments and policymakers worldwide.”
This is the first truly global picture of the wide inequalities in care for women’s cancers. Why did it take so long for this type of research to be conducted? What has been the biggest challenge for you, the researchers, and do scientists interested in this field have sufficient financial resources?
Claudia Allemani: Analyses of data from population-based cancer registries are key to plan and monitor cancer control strategies. Unfortunately, funding for population-based cancer research continues to be quite limited. The European Research Council Consolidator Grant was crucial to conduct this study because it allowed salaries for team members at LSHTM, as well as financial support for cancer registries in LMICs that wouldn’t have been able to collect detailed data on stage and treatment otherwise.
Data collection for all cancer patients diagnosed in the territory covered by each registry (province, state, region, or the whole country) takes time and expertise. The same is true for centralized data quality control and analysis to produce indicators of consistency with clinical guidelines that are truly comparable between countries worldwide. However, this standard process was substantially delayed by the amount of time we needed to spend finalizing the legal contracts to allow the transfer of funds for new data collection from primary medical records by selected cancer registries in 11 LMICs.
Access to data has also become increasingly difficult in high-income countries. We had to complete data-sharing agreements with many cancer registries in seven EU member states, Canada, and the US, to enable secure transmission of anonymized but sensitive personal data in compliance with the General Data Protection Regulation (GDPR) or similar laws and regulations. This has been an extremely time-consuming exercise, arguably not the best use of scientists’ time, especially because it does not take into account GDPR Article 9(2)(i), which permits the processing of anonymized individual records for public health research. Brexit also did not help.
We called for data in December 2019, and ideally, we would have received these data by the end of 2020 or early 2021. As you can imagine, all the processes mentioned above had been further complicated by the disruption caused by the COVID-19 pandemic during 2020–2022, which affected various areas of the world at different times.
How can these results be translated into practice so that the benefits are actually realized?
Claudia Allemani Our findings highlight several key messages for governments and policymakers worldwide. Prompt access to optimal treatment for breast, cervical, and ovarian cancers was available in most countries for early-stage tumors; therefore, efforts to promote improvement of early cancer detection should continue, both in HICs and LMICs. An increased number of radiotherapy centers and trained staff in LMICs, together with an increase in the coverage of public health insurance to include radiotherapy for economically disadvantaged women in some HICs, would improve consistency with treatment guidelines involving radiotherapy. International agreement on clinical guidelines is crucial, but they need to be tailored to local needs and resources, simplified, and made available in local languages.
Despite the delays caused by the COVID-19 pandemic, Brexit, and political or administrative issues in some LMICs, the VENUSCANCER project has demonstrated the feasibility of creating the first worldwide population-based database that includes detailed data on the clinical-therapeutic pathway, as well as bio-molecular information, collected by over 100 population-based cancer registries in both HICs and LMICs.
These data are essential to monitor consistency with clinical-therapeutic guidelines and to set recommendations for future cancer policies. Financial support from governments would ensure that these data are collected routinely by cancer registries. Long-term financial and political support for cancer registries should be a key priority for any government that wishes to implement and maintain a robust strategy for cancer control. Policymakers should also ensure that international regulations on data protection are not misinterpreted to compromise access to anonymized individual data, which are crucial for rigorous public health research.
The proportion of women with cancer who are diagnosed at an early stage is still far too low
What changes do you think these results should drive over the next year?
Claudia Allemani Treatment that is consistent with established international clinical guidelines for standard care still varies worldwide; however, it’s encouraging to see that if women are diagnosed early, prompt access to optimal treatment, such as life-saving surgery, for breast, cervical, and ovarian cancers has become more accessible for early-stage tumors in most countries. But this only helps if cancer is detected early enough. Sadly, the proportion of women with cancer who are diagnosed at an early stage is still far too low, especially in low- and middle-income countries. Efforts to promote early detection should continue in the years ahead. Early detection should not be limited to screening programs but should aim to improve cancer awareness in women as well as the efficiency of the clinical-therapeutic pathways, from detection of onset symptoms to prompt referral for optimal treatment in specialized hospitals.
Participation in screening programs is often low in LMICs and in more deprived regions in HICs due to women’s socio-economic status, lack of education, as well as distance from screening centers in rural areas. Non-specialized doctors should also be trained to recognize early symptoms promptly. Mobile screening units may also help increase participation. For cervical cancer, the HPV vaccine will help prevent cervical cancer in future generations. This vaccine targets teenagers, so education of young girls since primary school may play an important role to educate the whole family on cancer prevention and the importance of early detection.
Cancer impacts women across all societies, regardless of income or geography, so projects like VENUSCANCER play a crucial role in improving care and outcomes for women worldwide. The findings not only reveal disparities in diagnosis and treatment but also provide a foundation for shaping more effective and equitable health policies.
Image: Pink October/UICC.org
The VENUSCANCER project collected data from countries and territories across all continents. In Africa, participating registries included Nigeria (Ibadan), South Africa (Eastern Cape), and Uganda (Kampala). In Central and South America, data were contributed by Brazil (Aracaju and Jahu), Colombia (Cali, Manizales, and Pasto), Cuba, Ecuador (Quito), Martinique, and Puerto Rico. In North America, registries from Canada (Alberta, Manitoba, New Brunswick, Newfoundland and Labrador, Prince Edward Island, and Saskatchewan) and the United States (Alaska, Greater Bay Area, Greater California, Idaho, Iowa, Kentucky, Los Angeles, Minnesota, Montana, New Jersey, New York, Seattle, and Utah) participated. Asian contributors included Georgia, Iran (Golestan), Jordan, Mongolia, the Occupied Palestinian Territory (Gaza), Singapore, South Korea, and Thailand (Chiang Mai and Lampang). Europe had numerous participating countries and regions, including Belgium, Denmark, Estonia, France (Bas-Rhin, Calvados, Côte-d’Or Gynaecologic, Doubs, Gironde General, Haut-Rhin, Haute-Vienne, Hérault, Isère, Lille Metro, Loire-Atlantique, Manche, Poitou-Charentes, Somme, and Tarn), Germany (Hamburg), Ireland, Italy (Emilia Romagna, Friuli-Venezia Giulia, Genoa, Milan, Naples, Palermo, Pavia, Ragusa, Siracusa, Torino, Varese, and Veneto), Liechtenstein, Luxembourg, the Netherlands, Norway, Portugal (north and south), Romania (Cluj), Russia (Arkhangelsk and Samara), Slovenia, Spain (Basque Country, Castellon, Girona, Granada, Murcia, Navarra, and Tarragona), Switzerland (East Switzerland, Geneva, Graubünden-Glarus, Neuchâtel, and Ticino), and the United Kingdom (England, Northern Ireland, and Scotland). In Oceania, Australia (Australian Capital Territory, Queensland, and South Australia) and New Zealand participated.