Europe Faces Urgent Challenge of Antimicrobial Resistance: Experts Call for Health Literacy and Stewardship
In a commentary published at the beginning of the year, the authors warn that antimicrobial resistance (AMR) requires an urgent and coordinated response from healthcare systems, governments, and citizens.
The commentary titled “Enhancing antimicrobial stewardship and health literacy in Europe – moving forward through education and empowerment” is authored by Gabor Kertes, Andrew Robertson, Lisa Ackerley, Maria Brink Liljeberg, Christina Swedmark, Adrian Shephard, Thomas Bosch, Anders Miki Bojesen, Jessica Carreño Louro, Michele Calabró, Dorota Sienkiewicz, Pikka Jokelainen, Marianne Bengtsson, Lisbeth Thyregod, Nina Sønderberg, Charan Nelander, and Lars Münter.
“The European Parliament – in the resolution on the Pharmaceutical Strategy for the EU – recognised antimicrobial resistance as a major global health problem and a serious risk to the well-being of European citizens that will pose a major challenge to European health systems and societies, and called on the EU to establish common therapeutic guidelines for antimicrobials,” the authors stated.
In Europe alone, AMR is associated with more than 670,000 infections annually
Antimicrobial resistance occurs when bacteria and other microorganisms develop the ability to survive despite the action of antibiotics. According to data highlighted by the authors, in Europe alone, AMR is associated with more than 670,000 infections annually, around 33,000 deaths, and economic losses of approximately €1.1 billion per year due to treatment costs and reduced productivity. One of the main causes of AMR development, the authors stress, is the inappropriate use of antibiotics. Antibiotics are often used to treat viral infections such as the common cold or most sore throats, even though they work only against bacteria. In such cases, antibiotics provide no benefit but can contribute to the development of bacterial resistance.
The commentary also highlights the importance of the human microbiome, the community of microorganisms living in our bodies. These bacteria play a key role in protecting the body from infections and maintaining overall health. When antibiotics destroy beneficial bacteria, the balance of the microbiome can be disrupted, allowing harmful bacteria to spread more easily. Changes in the microbiome have been linked to various health problems, including chronic diseases and immune system disorders.
Health literacy and responsible antibiotic management
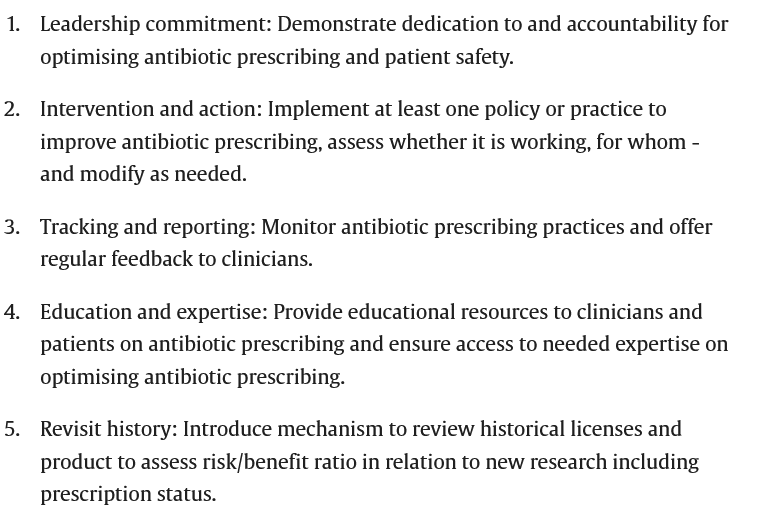
The authors particularly emphasise the urgent need to strengthen antimicrobial health literacy and responsible antibiotic management. They highlight the importance of health literacy alongside the implementation of antimicrobial stewardship systems.
They also explained the importance of the “One Health” approach, which links human, animal, and environmental health. Antibiotics used in livestock farming and agriculture can enter soil and water systems, promoting the development of resistant bacteria. “Industrial impact has been identified as one of the major causes of AMR spread, for example, through the release of active antimicrobial compounds into the environment. Monitoring hospital wastewater and other industrial pathways could therefore be a specific point of focus,” the authors explained.
“The AMR challenge is well recognised but addressed with too little action”
In a globalised world, resistant bacteria can spread rapidly between countries and continents. The authors warn that while AMR is widely recognised as a major challenge, too little concrete action is still being taken to address it. “The AMR challenge is well recognised but addressed with too little action,” they wrote.
The authors particularly stress the need for additional investment in health literacy and in strengthening citizens’ ability to practice self-care. Alongside organisational measures, educational activities targeting the public are essential to help people better understand when antibiotics are needed and when they are not. One particularly concerning issue highlighted in the commentary is the availability of antibiotics without prescription in some countries. The solution lies in stricter regulation and consideration of transitioning to systems where antibiotics are available only with a medical prescription. Infection prevention is also a key element in tackling AMR. Improving hygiene, indoor air quality, and education on infection prevention can significantly reduce the need for antibiotics.
They warn that combating antimicrobial resistance requires joint action from all parts of society. “We encourage healthcare professionals, health communication professionals, decision-makers, and civil society to strengthen their joint commitment to collaboration and action through systemic measures, dedicated antibiotic stewardship, and improved health literacy, including stronger evidence-based self-care, in order to help address the AMR challenge,” the authors concluded.
Image: Antibiotics and Antibiotic Resistance, McFarlandClinic