AI Predicts Interval Breast Cancer Risk
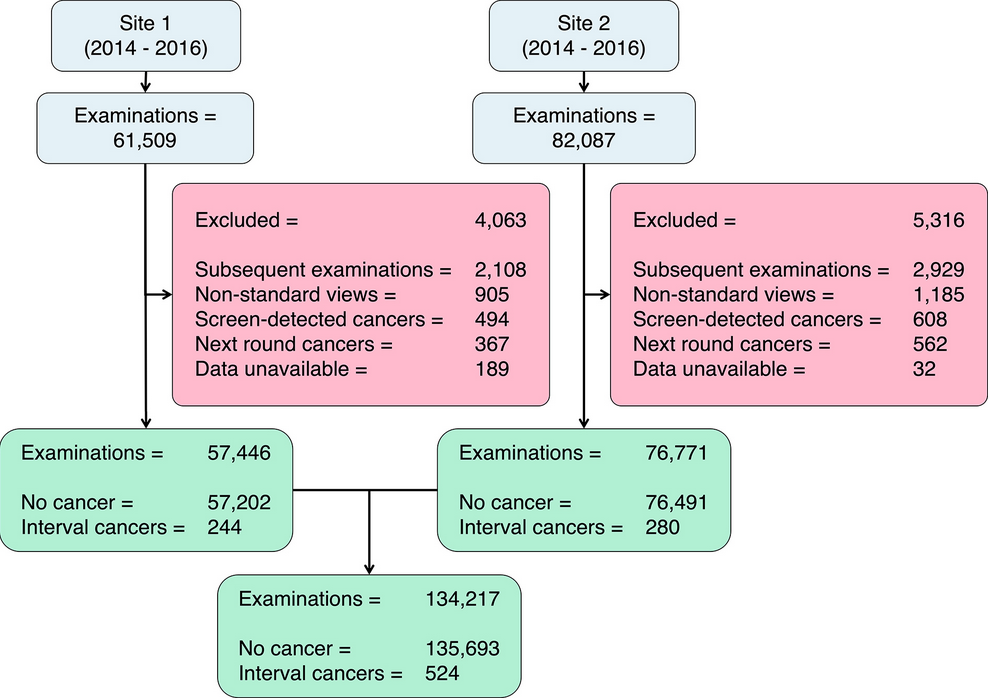
A new study conducted on more than 100,000 screening mammograms, more precisely 134,217, showed the importance of artificial intelligence tools in helping identify women at higher risk of developing interval breast cancer.
Scientists investigated the potential of applying deep learning to personalized breast cancer screening in the United Kingdom, where women aged 50 to 70 are routinely invited for mammograms every three years. The study used Mirai, an artificial intelligence algorithm that analyzes digital mammograms and estimates the risk of developing interval breast cancer, that is, cancer that is diagnosed between regular screenings and usually has a worse prognosis due to later detection. MIRAI was developed by a team of researchers at MIT and Massachusetts General Brigham.
“Mirai’s performance was also considered for different age quartiles and Breast Imaging Reporting and Data System (BI-RADS) (18) breast densities, as increased density is known to reduce screening mammography sensitivity…For this retrospective study, Mirai processed digital screening mammograms with negative results collected from a 3-year cohort (January 2014 to December 2016) across two sites and two primary mammography systems,” the authors wrote.
The results of the study, Evaluation of a Mammography-based Deep Learning Model for Breast Cancer Risk Prediction in a Triennial Screening Program, were published at the end of October 2025. Collaborating with Dr. Gilbert and Joshua Rothwell were Priya Rogers, M.B.B.S., M.Phil., Nicholas R. Payne, Ph.D., Yuan Huang, Ph.D., Josh D. Kaggie, Ph.D., Sarah E. Hickman. M.B.B.S., Ph.D., Fleur Kilburn-Toppin, M.B.Ch.B., Bahman Kasmai, M.Sc., and Arne Juette M.B.Ch.B.
We spoke with co-author Fiona J. Gilbert, M.B.Ch.B, Professor of Radiology at the University of Cambridge, United Kingdom.
The AI tool was more accurate at predicting interval cancers
The AI tool primarily uses information from mammograms, including breast density and subtle imaging features, to predict a woman’s risk of developing breast cancer. In this study, the model’s 3-year risk scores were evaluated retrospectively. It correctly identified 3.6% (19/524), 14.5% (76/524), 26.1% (137/524), and 42.4% (222/524) of 524 interval cancers among women with the highest 1%, 5%, 10%, and 20% of predicted risk, respectively. In other words, the AI tool was more accurate at predicting interval cancers that appeared within the first year after screening than those that developed 12–24 or 24–36 months later, and its performance was slightly reduced in women with extremely dense breast tissue compared with conventional risk prediction tools.
“We will need to secure funding for a prospective trial…”
As stated, next steps for the researchers include comparing commercially available predictive AI tools, conducting economic modeling and a cost-effective analysis, and conducting a trial utilizing predictive AI to identify women most likely to benefit from supplemental breast imaging following screening mammography.
How long might this last?
Fiona J. Gilbert: We are conducting a comparison of existing predictive AI mammography tools at the moment. We have held a stakeholders meeting to decide how best to proceed in the UK. We will need to secure funding for a prospective trial to be run within the national breast screening program. This might take the form of an in-service evaluation.
What is the crucial step? What kind of support is most needed?
Fiona J. Gilbert: We need to publish the second paper comparing the tools and then prepare a grant application to fund the prospective study. We also need to demonstrate that clinically important interval cancers can be found earlier – ie, grade 2 and 3 interval cancers. Funding and the engagement of policymakers are required to demonstrate that this method is better than density for improving early detection of cancer.
According to data from 1,000 women screened for breast cancer, 8 are diagnosed with cancer, 992 receive a normal result, and approximately 3 of these will develop interval cancer. In England, around 6,000 women develop interval cancer each year.
Image: Mammography/FDA.GOV
Patient-friendly information on mammography: RadiologyInfo.org.