The role of visceral fat in endometrial cancer
“This year marks a significant milestone for our association as we celebrate four decades of pioneering advancements and collaborative efforts in the field of nuclear medicine. Our congress will be a unique opportunity to reflect on our journey, celebrate our achievements since 1985, and look ahead to securing the brightest future for our specialty. The EANM Annual Congress is a truly global event, attracting about 10,000 participants from all over the world.”
With these welcome words, Dr. Valentina Garibotto, EANM Congress Chair 2023–2025, set the tone for the congress, celebrating past achievements while inspiring continued collaboration and innovation across the international nuclear medicine community.
Since its founding in 1985, the European Association of Nuclear Medicine (EANM) has grown into Europe’s leading non-profit medical organization dedicated to the development and advancement of nuclear medicine. For more than four decades, EANM has promoted innovation, fostered knowledge exchange, and strengthened collaboration among professionals. Its annual congress has become one of the most important global gatherings in the field, attracting nearly 9,000 participants from a wide range of medical specialties and countries.
This year, the congress took place in Barcelona, the historic city where the renowned Spanish Nobel laureate Santiago Ramón y Cajal made his remarkable contributions to science. All topics and research presented at the congress can be explored in the EANM’25 Abstracts Book, which is freely available online.
It was at this congress that medical physicist MSc. Jostein Sæterstøl, who has more than 15 years of experience in the field of nuclear medicine, presented his research. MSc. Sæterstøl recently began his doctoral studies at the University of Bergen, working at the Mohn Medical Imaging and Visualization Center at Haukeland University Hospital. His study reveals that metabolically active visceral fat may be associated with more aggressive forms of endometrial cancer. He is also one of the authors of the study, “Abdominal fat distribution in endometrial cancer: from diagnosis to follow-up,” which was published in May of this year.
Endometrial cancer and visceral fat
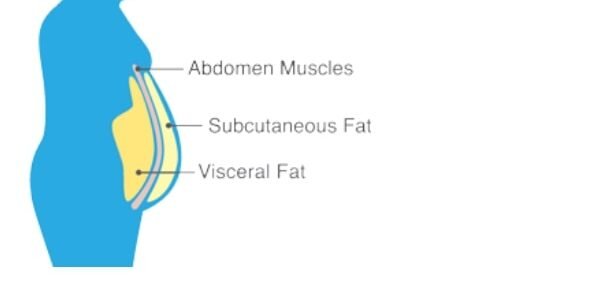
Endometrial cancer is the sixth most common cancer among women worldwide, with 420,368 new cases reported in 2022. Obesity is a well-established risk factor for endometrial cancer. Obese people often have increased amounts of visceral fat, the fat that accumulates around internal organs. Unlike subcutaneous fat, visceral fat is metabolically active and produces hormones and inflammatory molecules such as cytokines. For this reason, higher amounts of visceral fat in obese people are associated with an increased risk of cardiovascular disease, diabetes, and certain types of cancer, including endometrial cancer.
A team of researchers from Haukeland University Hospital and the University of Bergen analyzed PET/CT scans of 274 women with endometrial cancer. Before the PET/CT scan, the patients were injected with a small amount of radioactive glucose (FDG, fluorodeoxyglucose), which behaves like regular glucose in the body. This allowed the researchers to measure how metabolically active the visceral fat was, or how intensively it used glucose. By combining PET and CT technology, the researchers obtained both functional and anatomical data. The results showed that women with higher metabolic activity were more likely to have an advanced stage of the disease and lymph node metastases.
As lead author Jostein Sæterstøl explained, higher metabolic activity in visceral fat tissue was significantly associated with advanced cancer stages and the presence of lymph node metastases. It is important to note, however, that the researchers did not observe a strong correlation between the volume of visceral fat tissue and its metabolic activity. As he explained, this suggests that it is not just about the amount of fat, but also about its biological activity.
As Sæterstøl pointed out, the association between higher visceral fat metabolism and aggressive disease is likely driven by multiple mechanisms. So we asked him whether all of these mechanisms are known. “The processes themselves are described, but much is still not known about the interplay between, e.g., the release of cytokines from visceral fat and the effect on endometrial cancer aggressiveness. The mechanisms we describe are possible contributors, but further studies are needed to conclude whether they are all equally important, or if some of them act as the main driver mechanism,” Sæterstøl said.
Visceral Fat Measurement and the Role of Hormones
As noted, measuring visceral fat metabolism with PET/CT is not yet ready for routine clinical use due to technical challenges and variability, especially given the low uptake signal in fat tissue.” Does that mean that if you can’t measure it, you can’t stop that metabolism? Is there a way to reduce that metabolism?
Jostein Sæterstøl: The issue we’re addressing in this sentence is related to the technical side and the generally low signal from fat. Because of the low uptake, as well as small differences and overlap in the values between patient groups, this measurement method is not ready for routine clinical use. With ‘clinical use’ in this setting, we are referring to the use of information from the pretreatment imaging to directly guide treatment, perform risk stratification, and aid in prognosis estimation. It is well known that having large amounts of visceral fat increases the risk of several diseases, and that reducing visceral fat can lead to a better prognosis. Lifestyle changes, including a healthy diet and regular exercise, are the best way to reduce visceral fat.
The study ”Exercise training reduces inflammatory metabolic activity of visceral fat assessed by 18 F-FDG PET/CT in obese women “ (not related to endometrial cancer) that investigated the effect of exercise on visceral fat metabolism concluded that their preliminary data “might support that exercise training could be a promising non-pharmacological strategy to reduce inflammatory activity of VAT [visceral adipose tissue].” However, there is not sufficient evidence to conclude that lifestyle changes specifically reduce visceral fat metabolism, but reducing the amount of visceral fat through lifestyle changes is known to be beneficial in several diseases.
To what extent can age and hormones influence this, and can any preventive advice be given based on these data?
Jostein Sæterstøl: The amount of visceral fat increases with age, and menopause is also associated with increased abdominal and visceral obesity. A study from our group found that estradiol levels in plasma were positively correlated with the percentage of visceral fat in a small cohort of endometrial cancer patients. Studying the association between visceral fat and hormones is a complex task, given that hormone levels change on a short time scale (e.g., with a 24-hour rhythm, with diet, and many other factors). Available data highlights the increased risks of e.g., cardiac disease, diabetes, and various cancers with obesity, and with large amounts of visceral fat. Prevention advice is focused on lifestyle changes. The same advice is relevant for the patient group in our study. But again, whether this advice would help reduce the actual visceral fat metabolism (not just the amount of visceral fat) has not been much studied.
Of course, additional research is needed to improve measurement methods and explore the relationships between these factors. Additionally, they plan to investigate whether temporal changes in visceral fat activity are associated with disease progression or treatment response.
Image: Visceral fat, Luxembourg Institute of Health