Contaminated Meat Behind Urinary Tract Infections
Escherichia coli causes a wide range of infections, including sepsis, and is associated with approximately one million deaths worldwide each year. Extraintestinal pathogenic strains of E. coli (ExPEC) are the primary cause of urinary tract infections (UTIs) outside the gastrointestinal tract; they are responsible for most of the estimated 6–8 million UTIs in the United States annually. While food-producing animals can serve as reservoirs for zoonotic ExPEC strains, distinguishing these from strains endemic to humans is challenging.
A new study found that one in five urinary tract infections in Southern California may be caused by strains of E. coli spread through contaminated meat, with people living in low-income neighborhoods at the highest risk.
The study, titled “Zoonotic Escherichia coli and Urinary Tract Infections in Southern California,” was published in October.
We spoke with Lance B. Price, the lead author of the study and a professor of environmental and occupational health at George Washington University. Professor Price is also the founder and director of the Center for Action on Antibiotic Resistance at the GW Milken Institute School of Public Health.
The study and the results
As researchers point out, the extraintestinal pathogen Escherichia coli is the leading cause of urinary tract infections worldwide and can be transmitted from food animals to humans through contaminated meat. However, the contribution of zoonotic strains in urban areas is unclear. So over a four-year period, more precisely from 2017 to 2021, they collected 12,616 E. coli isolates from retail meat and 23,483 from patients with urinary tract infections, sequencing a representative subset of 5,728 isolates. The research focused on eight Southern California counties.
The majority of patients with UTIs were women—88%—with a median age of 50 years; 37% were Hispanic and 31% were non-Hispanic. Zoonotic strains accounted for about 18% of all urinary tract infections.
The study results showed that the highest proportion of zoonotic ExPEC isolates was identified among patients residing in areas with high poverty rates, 21.5% of all clinical E. coli isolates, and lower proportions of zoonotic ExPEC isolates were found in areas with medium (17.5%) and low (16.6%) poverty rates. After adjusting for age, sex, and race/ethnicity, individuals residing in a high-poverty area had a 1.6-fold increased risk of zoonotic ExPEC infections compared to those in low-poverty areas. Also, women had a higher zoonotic proportion than men, 19.7% vs 8.5%. As stated in the study, these results highlight the contribution of zoonotic ExPEC to the burden of urinary tract infections in Southern California and the need for targeted interventions to reduce risk in vulnerable communities.
“In 2023, we described a novel statistical-genomic model for inferring the host origin of E. coli strains based on both core-genome phylogeny and mobile genetic elements (MGEs) differentially associated with food animals and humans. In the current study, we applied this Bayesian latent class model to a large contemporaneously collected set of E. coli isolates from retail meat and humans with UTIs in Southern California,” they wrote in the study.
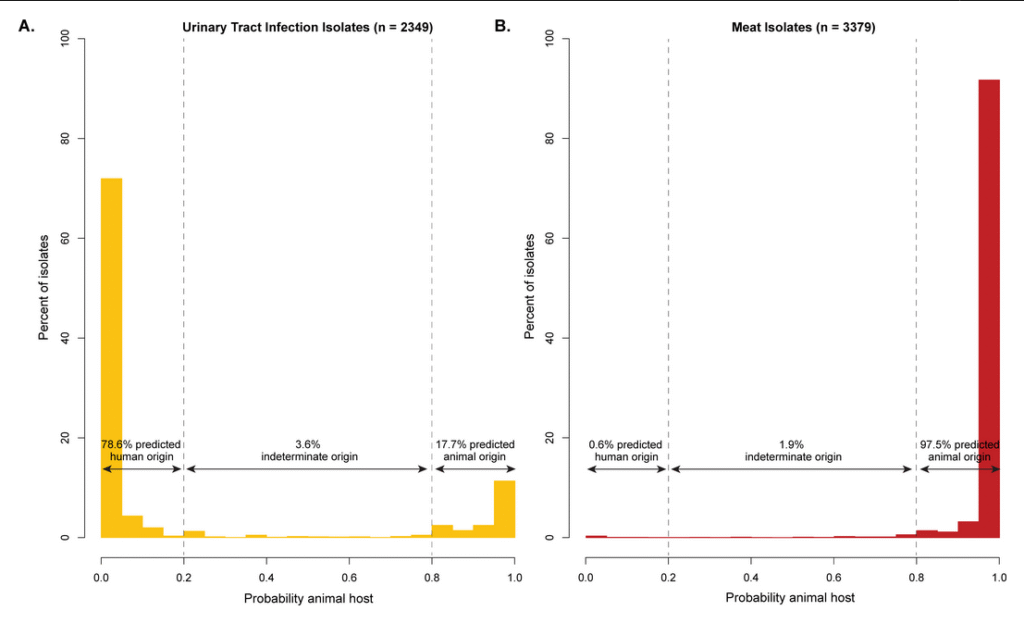
“Zoonotic ExPEC-associated sequence types were most common in isolates from retail chicken (38%) and turkey (36%), followed by beef (14%) and pork (12%). A small subset of E. coli lineage from meat was disproportionately responsible for a large portion of the ExPEC strains identified in human clinical urine samples, suggesting that these virulent animal-associated strains represent the greatest zoonotic risk.”
How might this affect antimicrobial resistance?
People in poorer communities are at greater risk, which may be due to meat contamination, poor storage conditions, inadequate hygiene, and food preparation methods; however, it is important to note that the factors underlying the strong correlation between poverty rate and zoonotic UTIs are unclear.
Additionally, zoonotic strains share similar antibiotic resistance patterns with meat-borne bacteria. When asked how this might affect antimicrobial resistance, Professor Price said: “In places where antimicrobial use in food animals is poorly controlled, this could mean more drug-resistant urinary tract infections in people.“
As for what surprised him most, Professor Price pointed to the 2023 study, noting that the proportion of zoonotic infections estimated in this Southern California population was about twice what had been found in a similar study in Flagstaff, Arizona. ”The rate was higher than I was anticipating based on our previous large-scale study in Arizona, but we have now looked at different datasets and see roughly the same rate in other high-income countries. In low- and middle-income countries, the rate may be significantly higher,” said Professor Price.
As they explain in the study, the overall proportion of antimicrobial resistance was comparable between the current study in Southern California and the previous study in Arizona, both for clinical isolates of E. coli (52.9% vs. 54.9%) and for isolates from meat (64.7% vs. 67.5%). In other words, the bacteria’s antibiotic resistance was roughly the same in both regions, in both human infections and meat, although the percentages were slightly different.
Protecting public health
Identifying this route of exposure presents new opportunities to reduce the burden of urinary tract infections. Scientists also point out that meat producers and regulatory agencies should consider stricter measures to limit the prevalence of ExPEC in retail meat, especially poultry. Regarding precautions, they note that people at increased risk of bacterial infections should be cautious when handling raw meat (including frozen); such measures, including hand washing, avoiding cross-contamination, and ensuring that meat products are properly cooked, are key to reducing exposure. “Addressing this overlooked pathway of ExPEC transmission is imperative for protecting public health and reducing the incidence of foodborne UTIs,” they concluded.
Image: Urinary tract infections/monash.edu
The research was supported by the Wellcome Trust, the National Institute of Allergy and Infectious Diseases, and the Johns Hopkins Sherrilyn and Ken Fisher Center for Environmental Infectious Disease Discovery Program.